Abstract
Antigen-specific regulatory T cells (Tregs) possess the potential to reduce excess of immune responses following allogeneic hematopoietic stem cell transplantation. Although antigen-specific in vitro- expanded Tregs (iTregs) have long been considered as a promising therapeutic agent against allo-immune reactions such as graft versus host disease (GVHD), accumulating evidences have suggested that iTregs easily lose their characteristics with quick cessation of Foxp3 expression , a lineage specifying transcription factor of Tregs, compared with in vivo -generated natural Tregs (nTregs). It has been revealed that insufficient demethylation of the CpG islands in conserved noncoding sequence 2 (CNS2) region of the Foxp3 locus mainly explains such instability of Foxp3 expression in iTregs.
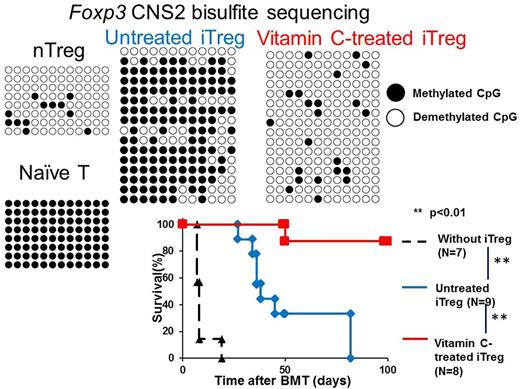
In order to overcome this drawback, we investigated the optimum way to generate stable iTregs for the prevention of a murine model of acute GVHD. We created a major-MHC mismatched GVHD model by transferring CD45.1 (H-2Kb) bone marrow (BM) cells together with effector T cells (CD4+25- and CD8 cells) into lethally irradiated (8Gy/body) 8-12-week old BALB/C (H-2Kd) recipients. In this model, recipient mice usually die within 7-10 days after bone marrow transplant (BMT) due to severe acute GVHD. Alloantigen-specific iTregs were generated by co-culturing naive T cells from human CD2 Foxp3 reporter mice (C57BL6/J background, H-2Kb) with BALB/C-derived antigen presenting cells in the presence of TGF-β, IL-2 and retinoic acid. Alloantigen-specific iTregs were then harvested 6-7 days after co-culture, by FACS-sorting the CD4+Foxp3+ population. Subsequently, sorted iTregs (106 cells) were transferred intravenously together with effector T cells (106 cells) and BM cells into recipients. We tested a panel of pharmacological agents and gene transduction during co-culture for their effects on iTreg stability, with FACS-based evaluation on day 7 after BMT. Among a panel of agents and gene modification tested, we found that only vitamin C-treated iTregs effectively improved Foxp3 maintenance compared with untreated iTregs (90%, vitamin C-treated iTregs vs 40%, untreated iTregs) in the GVHD model mice. As reported, vitamin C facilitated DNA demethylation of the Foxp3 CNS2 in iTregs in a Tet DNA demethylase-dependent manner. Bisulfite sequencing revealed a significant acceleration of CpG demethylation at the Foxp3 CNS2 by vitamin C, and the extent of demethylation achieved with vitamin C treatment reached to an equivalent level to those seen in nTregs. Furthermore, vitamin C mediated demethylation was extended to other Treg cell-specific regulatory lesions such as Tnfrsf18, Ikzf4, Ctla4 . On the other hand, untreated iTregs remain methylated at these loci to the same degree as naïve T cells (p<0.05) . At the same time, interestingly, production of inflammatory cytokines such as IFNγ and IL-21 that was observed in untreated iTregs which lost Foxp3 expression (ex- Foxp3 iTreg) was not observed in vitamin C-treated counterparts. Additionally, we further evaluated the benefits of vitamin C treatment, by investigating effects of another well-known demethylating agent, 5-aza-2'-deoxytidine (5-aza-dC). As a result, 5-aza-dC did not only induce DNA demethylation of Foxp3 CNS2, but also of the CNS1 enhancer region of the inflammatory cytokine IFNγ locus, even in iTreg conditioning culture. This nonspecific demethylation was not observed in vitamin C-treated iTregs (p<0.01). Finally , adoptive transfer of vitamin C-treated iTregs ameliorated GVHD in mice. Vitamin C-treated iTreg prolonged survival at BMT day 45 compared with untreated iTreg (100%, N=8, vitamin C treated iTreg group, vs 44.4%, untreated iTreg group, N=9, p<0.01). Amelioration of acute GVHD by vitamin C-treated iTreg was also confirmed by colon length on day 7 after BMT (p<0.05) and pathological findings of colon and small intestine.
In summary, vitamin C stabilized Foxp3 expression with specific demethylation of Foxp3 CNS2 as well as Treg-associated genes in antigen-specific iTregs, preventing them from conversion into inflammatory ex- Foxp3 iTregs, thus ameliorating the pathogenesis of a murine model of GVHD. Our findings strongly suggest the potential of clinical application of Treg therapy combined with vitamin C treatment, for GVHD and autoimmune diseases.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal